1. INTRODUCTION
- All animals (acellular and multicellular) need the continuous supply of oxygen and nutrients (transport) for their life activities. There is also the need for the removal of waste products from them (execretion) for the normal functioning of the body. As such it is essential for the development of a transport mechanism to serve the above two functions. We find different transport mechanisms in different groups of animals.
- In acellular animals like Ameoba, Paramecium, there is no need for a transport mechanism as the body is in direct contact with the surrounding water medium. The streaming movements of the cytoplasm in the cells facilitates circulation of substances and elimination of waste products.
- Simple organisms such as sponges and cnidarians circulate water drawn from their surroundings through their body cavities facilitating exchange of substances.
- More complex organisms use special ‘circulatory fluids’ within their bodies to transport different materials.
- Blood and lymph together constitute the fluid tissues
- Blood is the most commonly used circulatory fluid by most of the higher organisms including humans.
2. LYMPHATIC SYSTEM
- It is an extensive network of thin – walled vessels that arise as blind ended lymph capillaries in most of the tissues of the body.
- The lymph capillaries unite to form a tree like structure of increasingly larger lymph vessels.
- Which finally drain lymph into veins in the lower neck region. Lymphatic system is an open circulatory system.
- Lymph capillaries are microscopic, closed ended tubes that form vast network in the intercellular spaces.
- The walls are composed of endothelial cells, with porous junctions, through which interstitial fluid/ extracellular fluid (ECF), proteins, microorganisms and absorbed fats can easily enter. Once the extra cellular fluid enters the lymphatic capillaries, it is referred to as lymph.
- The lymph capillaries merge and form large, lymphatic vessels which lead into larger lymph ducts.
- The walls of the lymph vessels and ducts are similar to those of veins and are provided with valves.
- The smooth muscles of their walls cause peristaltic waves of contraction pushing lymph towards the neck region.
- All the lymph vessels from the lower part of the body eventually empty lymph into the thoracic duct.
- The thoracic duct of the lymphatic system is the largest lymphatic vessel (lymph duct) in the body.
- It is also known as the left lymphatic duct, chyliferous duct . Lymph collected from the left side of the head, neck ,the left arm, and the parts of the chest region also enters the thoracic duct before it empties into the venous system at the junction of the left subclavian vein and internal jugular vein.
- Lymph from the right side of the neck, head, right arm, and the right part of the thorax is collected into the right lymphatic duct which empties it into venous system at the junction of the right subclavian vein and internal jugular vein.
- Thus, lymph, which was once a part of the blood that came out of the blood vessels to supply oxy-gen and nutrients to tissues, as the ECF, is finally drained back into the left and right subclavian veins (venous system).
- Before lymph is returned to the heart via the venous system, bacteria, viruses etc., are phagocytised by the WBC in the lymph nodes.
- The lymphatic system also consists of other organs such as spleen, thymus, tonsils etc. MALT and appendix also constitute a part of the lymphatic system.
- Spleen is the largest lymphatic organ and is also the reservoir of red blood cells/ blood and lymphocytes. It acts as ‘haemopoietic organ’ until the fifth month of gestation.
Formation of lymph
- When blood passes through the capillaries, due to high filtration pressure at the arteriolar ends of capillaries, along with plasma, many substances such as glucose, small sized organic molecules, inorganic salts etc. (except the large plasma proteins) are filtered into the extracellular spaces where it is called “tissue fluid/ ECF”.
- This causes an increase in colloidal osmotic pres-sure of the plasma (due to plasma proteins).
- This pressure favours the movement of about 85 percent of the ECF into the capillaries at the venular ends after exchanging oxygen, CO2, nutrients, other metabolites etc., with the tissues.
- The remaining 15% of ECF is collected into the lymphatic system through lymph capillaries. Henceforth it is called lymph.
- In a pregnant woman when the enlarged uterus exerts pressure on the abdominal veins, thus increase the capillary hydrostatic pressure, it leads to accumulation of fluids (ECF) in the legs, hence the swollen legs – ‘edema’, in them.
Composition of lymph
- Lymph is similar in its composition to the blood’s plasma, except that it contains a much lower concentration of proteins and other nutrients than plasma.
- Erythrocytes are absent. Lymph contains water, some plasma proteins, electrolytes, leucocytes mostly lymphocytes.
- Some coagulation factors, antibodies, enzymes, nutrients etc. An emulsion of lymph and triglyceride fat (chylomicrons_), characteristically present in lacteals is called chyle.
Functions of lymphatic system 1. Lymph returns the absorbed nutrients and wastes from the body parts to the blood 2. It transports lymphocytes from the lymphatic glands to the blood 3. It transports digested fats which are absorbed through lacteals, present in the intestinal villi to the blood vascular system. 4. It destroys the invading microorganisms and foreign particles in the lymph nodes. 3. CLOTTING OF BLOOD
- Clotting is a complex cascade of enzymatic reactions in which each clotting factor activates many molecules of the next one in a fixed sequence
- Clotting of blood is also known as haemostasis
- Calcium ions play a very important role in clotting in both pathways
- Breakage of a blood vessel exposes collagen proteins to the blood, which can initiate clotting 1. vasoconstriction, 2. platelet plug formation or 3. clot formation
- Clotting takes place in three essential steps
- In step 1, Prothrombin activator is formed by a complex cascade of chemical reactions in intrinsic or extrinsic pathways
Step I
- It involves the formation of a complex of activated substances collectively called prothrombin It is released in two path ways.
- Intrinsic pathway : It occurs when the blood is exposed to collagen of injured wall of blood vessel. This activates Factor XII, and in turn it activates another clotting factor, which activates yet another reaction (cascade fashion), which results in the formation of the prothrombin activator
- Extrinsic pathway : It occurs when the dam-aged vascular wall or extra vascular tissue comes into contact with blood. This activates the re-lease of tissue thromboplastin, from the damaged tissue. It activates the factor VII. As a result of these cascade reactions, the final product formed is the prothrombin activator
Step II
- The prothrombin activator in the presence of Ca ions, causes the conversion of inactive prothrombin to active thrombin.
Step III
- Thrombin converts the soluble protein fibrinogen into soluble fibrin monomers, which
- are held together by weak hydrogen bonds. The fibrin stabilizing factor replaces hydrogen bonds with covalent bonds to form a meshwork by cross linking the fibers. which helps in closing the wound.
- The insoluble mesh work of fibrin fibres spreading in all directions adhere to the damaged surfaces and trap the blood cells and platelets.
- The clot begins to contract so that the fluid is expelled out. This is called clot retraction.
- The fluid that is expelled out during clot retraction is serum.
Clotting Factors
| FACTOR | NAME |
| I | Fibrinogen |
| II | Prothrombin |
| III | Thromboplastin |
| IV | Calcium ions |
| V | Proaccelerin |
| VII | Proconvertin |
| VIII | Antihaemophic globulin |
| IX | Chirstmas factor |
| X | Stuart – prower factor |
| XI | Plasmathromboplastin antecedent |
| XII | Hageman’s factor |
| XIII | Fibirin stabilizing factor |
Note : Factor VI is no longer referred Anticoagulants
- Heparin is an anticoagulant synthesized by the mast cells and basophils.
- Heparin activates antithrombin, a plasma protein, which combines with thrombin and inactivates it.
- Coumarins of plant origin are the precursors of anticoagulants such as warfarin, which are antagonistic to vit-K and thus prevent the synthesis of clotting factors.
- Vitamin K is essential for the synthesis of clotting factors II, VII, IX and X in the hepatocytes of liver
- Clotting of blood in blood banks can be prevented by the addition of citrates or oxalates of sodium or EDTA.
- Haemolysin in the saliva of mosquitoes and hirudin in the saliva of leeches also act as anticoagulants.
4. CIRCULATORY PATHWAYS
- Circulatory patterns are open and closed types
- In open type, blood pumped by the heart passes through large vessels into the open spaces or cavities called sinuses
- In the open type of circulation, there is no distinction between the circulating fluid (blood) and the extracellular fluid of the body (interstitial fluid). This fluid is thus called Haemolymph.
- Open type of circulation is seen in leeches, arthropods, majority of molluscs, echinoderms and ascidians.
- In the closed circulatory system, the circulating fluid or blood, is always enclosed with in blood vessels that transport the blood away from and back to a pump, the heart.
- Closed circulation is seen in annelids, cephalopods, cepholochordates and all vertebrates.
5. PLAN OF CIRCULATORY SYSTEM IN THE VERTEBRATES
- Fishes have a 2-chambered heart with an atrium and a ventricle
- Heart of a fish is branchial heart. As blood passes through heart only once in a complete circuit, hence called single circulation
- Amphibians have a 3-chambered heart with two atria and one ventricle
- Reptiles have two atria and an incompletely divided ventricle (except crocodile)
- In amphibians and reptiles oxygenated and deoxygenated blood get mixed up in the single ventricle
- Amphibians and reptiles show an incomplete double circulation
- Birds and mammals possess a 4-chambered heart with two atria and two ventricles.
- In homeotherms, two completely separated circulatory pathways namely systemic and pulmonary circulations are present. Hence, these animals are said to be showing ‘double circulation’
6. HUMAN CARDIO-VASCULAR SYSTEM It consists of a four chambered muscular heart, a network of closed branching blood vessels and blood Structure of The Heart
- Heart is mesodermal in origin
- Situated in the mediastinum, slightly tilted to the left.
- Heart is covered by a double walled pericardium which consists of the outer fibrous pericardium and the inner serous pericardium
- The serous pericardium is double layered, formed of an outer parietal layer and an inner visceral layer.
- The two serous layers are separated by a narrow paricardial space, which is filled with the pericardial fluid
- The wall of the heart consists of an outer epicardium, the middle myocardium and the inner most endocardium. It directs the blood to the left atrium through foramen ovale.
- Heart has four chambers with two upper atria and two larger lower ventricles
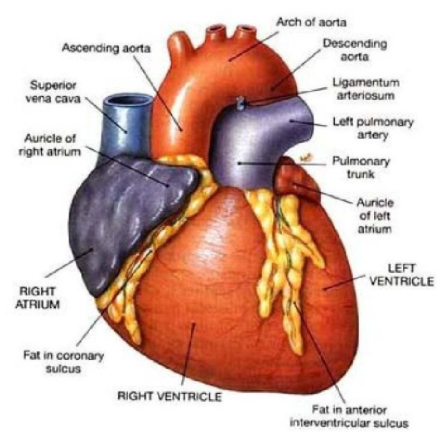
- Atria and ventricles are separated by a transverse coronary sulcus.
- The muscular pouch like projection from each atrium is called auricular appendix.
- Externally the ventricles are separated by two inter ventricular grooves, in which the coronary arteries and their branches are lodged.
Internal Structure 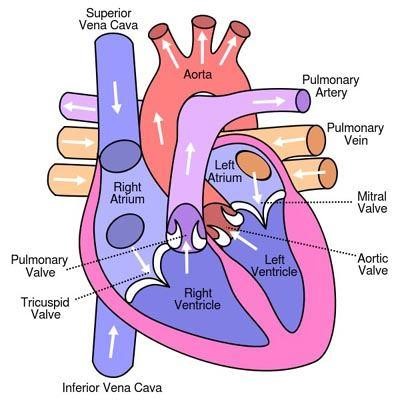
- Atria are thin walled receiving chambers
- Two atria are separated by an inter-atrial septum. It has a small pore called foramen ovale.
- Foramen ovale colses at birth, when lungs become functional.
- The right atrium receives deoxygenated blood from different parts of the body (except lungs) through two caval veins.
- The opening of post caval vein is guarded by the
Eustachian valve
- Eustachian valve becomes rudimentary and non-functional in adults.
- Right atrium also receives blood from myocardium through coronary sinus, whose opening into the right atrium is guarded by the valve of Thebesius.
- The left atrium receives blood from lungs through four pulmonary veins.
- Atria and ventricles are separated by atrioventricular septum, which possesses left and right atrioventricular apertures.
- The left and right apertures are guarded by bicuspid (mitral valve) and tricuspid valves
- Ventricles are the thick walled blood pumping chambers separated by an interventricular septum.
- The inner wall of the ventricles is raised into muscular ridges called columnae corneae.
- Some of the ridges are large and conical, and are called papillary muscles, whose apices are connected to the chordae tendineae.
- Chordae tendineae are cord-like collagenaous processes that connect the papillary muscles to the cuspid valves. They prevent the cusps of the AV valves from bulging too far into the atria during ventricular systole
Nodal Tissue 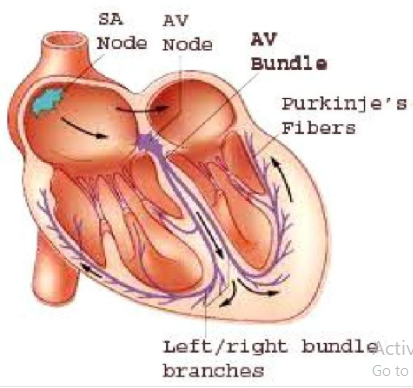
- It is the specialised cardiac musculature distributed in the heart.
- A patch of nodal tissue called the sinoatrial node (SAN) is present in the right upper corner of the right atrium near the opening of superior venae cavae.
- Another mass of nodal tissue, called the atrioventricular node (AVN) is seen in the lower left corner of the right atrium close to the atrioventricular septum.
- A bundle of nodal fibres, called atrioventricular bundle continuous from the AVN into the inter ventricular septum. It divides into right and left bundle branches.
- Bundle branches give rise to minute fibres called Purkinje fibres that extend throughout the ventricular musculature.
- SAN can generate maximum number of action potentials, i.e., 70-75 m–1 , and is responsible for initiating and maintaining the rhythmic contractile activity of the heart.
- Our heart normally beats 70-75 times in a minute (average 72 beats m–1 )
Aortic Arches
- Pulmonary arch arises from the right ventricle.
- Its opening is guarded by Pulmonary valve.
- Systemic arch arises from the left ventricle. Its opening is guarded by aortic valve (Pvt.)
- The pulmonary and aortic valves are made up of three semilunar flaps, each
- A fibrous strand known as ligamentum arteriosum is present at the point of contact of systemic and pulmonary arches. It is the remnant of the ductus arteriosus of embryonic stage.
7. CARDIAC CYCLE
- The cardiac events that occur from the beginning of one heart beat to the beginning of the next constitute a cardiac cycl
- Cardiac cycle consists of three phases namely atrial systole, ventricular systole and cardiac diastole
- Before the beginning of atrial systole, all the four chambers of heart are in a relaxed rate.
- Under normal condition, blood continuously enters the right atrium through vena cavae and left atrium through pulmonary veins. From the atria nearly 70% of the blood passively flows into the ventricles
- During the atrial systole (0.1 sec) cuspid valves are open and rest of the ventricular filling (30%) takes place.
- Now both ventricles contract (ventricular systole for 0.3 sec) which results in the increase of ventricular pressure, and both the atrioventricular valves are closed (causes lub sound) and semilunar valves open.
- Blood is now pumped through pulmonary artery to the lungs and through the aorta to the rest of the body
- The atria relax, although the ventricles are still contracted. Blood enters the atria from the large veins coming from the body.
- The ventricular systole is followed by the ventricular diastole during which, there is a fall in
- ventricular pressure
- The semilunar valves at the base of aorta close to prevent the backward flow of blood into the
- aorta (causes dup sound)
- As the ventricular pressure declines further, the AV valves are pushed open by the pressure in
- the atria exerted by the blood. The blood now once again flows freely into the ventricles
- All the heart chambers are now again in a relaxed state (joint diastole last for o.4 sec) soon another cardiac cycle sets in
- Human heart beats 72 times per minute normally.
- Hence the duration of a cardiac cycle is about 0.8 sec.
- The volume of blood pumped out by each ventricle for each beat is known as stroke volume
- The volume of blood pumped out by the heart for each ventricle per unit is formed cardiac output
- cardiac output = stroke volume of beats
- cardiac output = 700 ml 72 beats / minute = 5040 ml / min
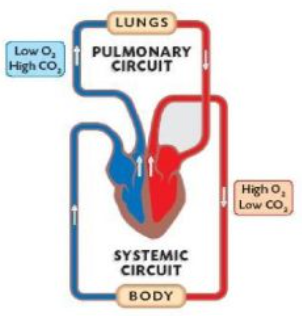
- The two main circulatory routes are the systemic and pulmonary circulations.
- In pulmonary circulation (lesser circulation), the blood pumped by the right ventricle enters the pulmonary artery
- The deoxygenated blood pumped into the pulmonary artery is passed on to the lungs from where the oxygenated blood is carried by the pulmonary veins into the left atrium
- Is systemic circulation (greater circulation) the oxygenated blood entering the aorta is carried by a network of arteries, arterioles and capillaries to the tissues from where the deoxygenated blood is collected by a system of venules, veins and vena cava and emptied into the right atrium.
- systemic circulation provides nutrients, O2 and other essential substances to the tissues and takes
- CO2 and other harmful substances away for elimination.
8. PORTAL CIRCULATION AND CORONARY CIRCULATION
- A blood vessel that starts in capillaries and ends in capillaries without reaching the heart is called a `portal vessel’
- There are 3 portal systems except in mammals
- A unique vascular connection exists between the digestive tract and liver which is called hepatic portal system. It carries blood from the intestine to the liver
- Renal portal system is present in all vertebrates except cyclostomes and mammals.
- The hypophyseal portal system links the hypothalamus and the adenohypophysis.
- A special coronary system of blood vessels present in our body exclusively for the circulation of blood to and from the cardiac musculature. It involves right and left coronary arteries and four cardiac veins
9. REGULATION OF CARDIAC ACTIVITY
- Normal activities of the heart are regulated intrinsically i.e., auto regulated by specialised muscles (nodal tissue) hence the heart is called myogenic
- A special neural centre in the medulla oblongata can moderate the cardiac functions through the `autonomic nervous system’
- Nerual signals from the cardiac accelaratory centre through the sympathetic nerves (Part of ANS) can increase the rate of heart beat, the strength of ventricular contraction and there by the cardiac output.
- Nerual signals from the cardiac inhibitory center through parasympathetic neural signals (another components of ANS) decrease the rate of heartbeat, speed of conduction of action potential and there by cardiac output.
- Adrenal medullary hormones,the epinephrine and norepinephrine can also increase the cadiac output Thyroxine also increases the heart rate and cardiac output.
10. BLOOD VESSELS
- Blood vessels form a tubular network throughout the body that permits blood to flow from the heart to all the living cells of the body and then back to the heart.
- The cardio vascular system has five general classes of blood vessels they are arteries, arterioles, capillaries, venules and veins.
- The large blood vessels, arteries and veins have essentially three layers in their walls . 1) Tunica exeterna or tunica adventitia consist of fibrous connective tissue, 2) Tunica media is made up of smooth muscles and 3) Tunica interna is made up of endothelium and basement membrane.
- In addition to the above layers arteries and arterioles have two elastic laminae one on either side of the muscular layer
- Veins have one elastic lamina inner to the muscle layer.
- The muscle layer is much thicker in the arteries than in the veins.
- Endothelium of veins is double folded to form valves.
- Capillaries are microscopic blood vessels through which materials are exchanged between blood and tissue cells
- A typical capillary consists of an endothelial tube inside a thin basement membrane
- Absence of smooth muscles and connective tissue layers in the wall of capillaries permits more rapid exchange of materials between the blood and the tissue.
11. DISORDERS OF CIRCULATORY SYSTEM Hypertension
- Blood pressure is the force exerted by the blood against the walls of the blood vessels
- Blood pressure is measured in the brachial artery of the arm by using a sphygmomanometer
- Pressure 120/80mm. Hg is considered normal blood pressure in human beings
- The upper reading pertains to systolic pressure and the lower one, the diastolic pressure.
- Blood pressure above 140/90 is considered as hypertension
- High blood pressure leads to heart diseases and also affects other vital organs such as the brain and kidneys
- Hypertension is generally treated by drugs that dilate blood vessels, drugs that increase the rate of urine production and drugs that decrease cardiac output
- Low salt diet is normally recommended to reduce the hypertension
DIFFERENCES BETWEEN ARTERIES AND VEINS
| CHARACTER | ARTERIES | VEINS |
| Location | Deep seated | Superficial |
| Wall | Thicker, more elastic | Thinner, less elastic |
| Tunica externa | Less developed | Thickest layer |
| Tunica media | Contains more smooth muscles and elastic fibres | Contains less muscles and fewer elastic fibres |
| Lumen (in section) | Narrower | Wider |
| Valves | Non-valvular | Valvular |
| Direction of blood | Away from the heart | Towards the heart |
| Rate of blood flow | Intermittent (Pulse) and fast | Slow and steady |
| Nature of blood | Oxygenated (except pulmonaryarteries) | Deoxygenated (except pulmonary veins) |
| Blood pressure | Higher | Lower |
| After death | Become empty | Contain blood |
| When empty | Retain their cylindrical shape | Collapse |
Coronary Artery Disease (CAD)
- CAD often referred to as atherosclerotic heart diseases
- It is caused by deposits of calcium, fat, cholesterol and fibrous tissue in the lumen of blood vessel
- This deposition makes the lumen of arteries narrow
- The narrow blood vessel reduces the blood flow to the heart, this leads to ischemia.
- Due to lack of oxygen myocardial cells may die, this is called myocardial infarction. Bypass surgery, balloon angioplasty, and use of stents can save the person’s life.
Angina Pectoris
- It is marked by chest pain caused by narrowing of blood vessels to the heart (Ischemia)
- Argina pectoris is a ‘warning signal’ of deprivation of blood supply to the heart muscles.
- It occurs in men and women of any age. but it is more common among the middle aged and the elderly people.
- The major risk factors for angina includes smoking, diabetes, high cholesterol, high blood pressure etc.
Heart Failure
- It is a condition in which the heart is unable to provide sufficient pumping action to distribute blood flow to meet the needs of the body.
- Common causes of heart failure include myocardial infarction or heart attack and other forms of ischemic heart diseases, hyper tension etc.
- It is also called congestive heart failure because of congestion of the lungs, which is one of the main symptoms of failure.








